Eighty-five percent of Americans have never heard of metabolic syndrome, a national health survey reported. And of the more than 211,000 people polled, only 0.6 percent thought they had it themselves. While that may make it sound extremely rare, metabolic syndrome affects 1 billion people worldwide, including 66 million Americans, prompting scientists to describe it as a “global epidemic.”
Although this lifestyle-linked malady is most common in older adults — affecting half of those over 60 — rates are soaring in younger adults, particularly those in their 20s and 30s, according to a recent study published in Journal of the American Medical Association. These are “alarming trends,” say the researchers, because if it goes undiagnosed and untreated, this disorder triples risk for heart attacks and more than quadruples it for type 2 diabetes. Here’s a closer look at metabolic syndrome and what you do to avoid it.
Only One in Eight Americans is Metabolically Healthy
Metabolic syndrome is a gang of cardiovascular bullies that attack in tandem, magnifying the threat of developing atherosclerosis (arterial plaque), fatty liver disease (fat buildup in the liver), obstructive sleep apnea, polycystic ovary syndrome, gallstones, several types of cancer and Alzheimer’s disease, which is 12 times more likely to strike people with the syndrome as those without it. Some scientists have suggested that metabolic syndrome be renamed “sitting disease,” since it’s most common in overweight or obese people with sedentary lifestyles.
Only one in eight Americans, however, is achieving optimal metabolic wellness, according to another new study. Researchers from the University of North Carolina (UNC) at Chapel Hill defined optimal metabolic health as meeting guideline-recommended targets for five factors — blood pressure, blood sugar, triglycerides, HDL (good) cholesterol and waist circumference — and not taking any medications related to these factors.
To determine how many Americans were at high vs. low risk for chronic illness, the team examined data from nearly 9,000 adult participants in the National Health and Nutrition Survey. The analysis found that only 12.2 percent of them were metabolically healthy, suggesting that nationally, only one in eight US adults are meeting optimal goals to protect their cardiovascular health and ward off chronic illness. The researchers also reported that 99 percent of the obese people studied were metabolically unhealthy.
A Dangerous Disorder You Can Diagnose Yourself
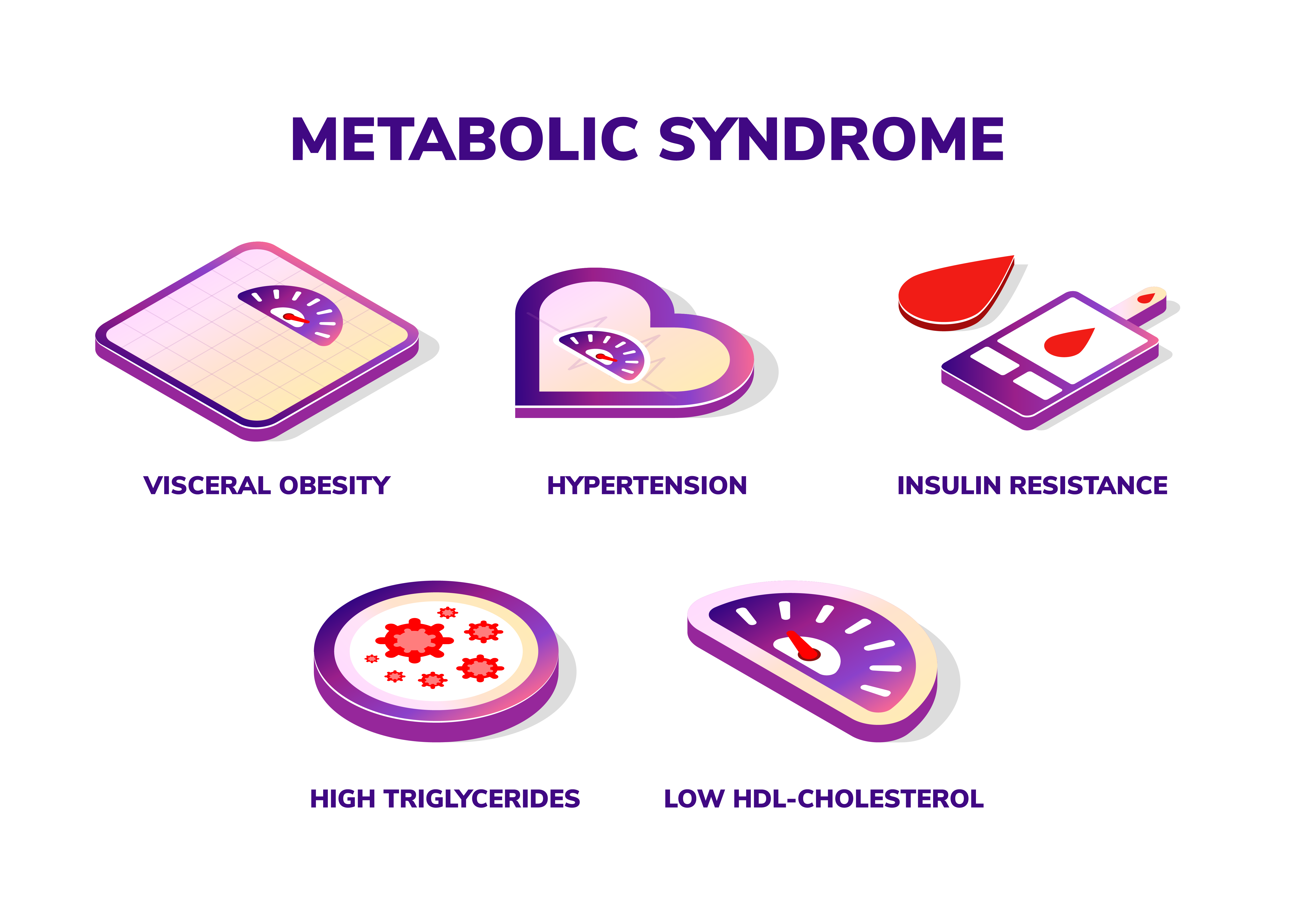
The good news is that metabolic syndrome is both preventable and highly treatable. You can find out if you have it simply by looking at a few basic numbers that should be in everyone’s health record. You should also be aware that it’s possible to have this condition even if you are not overweight, since the key driver is abdominal obesity, not overall fat. To make the diagnosis, check the following list of five warning signs. Making the call is a little like baseball: Three strikes and you’re out, since having at least three of these factors means that you have metabolic syndrome. If so, we’ve included some action steps to address the various risk factors.
- A large waist. Up to 70 percent of people with the syndrome are saddled with excessive belly fat, giving them an apple shape. Sometimes called “middle-aged spread,” this type of fat is metabolically active, releasing compounds that contribute to chronic inflammation, insulin resistance and high blood pressure, all of which increase your risk for CVD and other chronic diseases. A waist measurement of 35 or more inches for a woman, or 40 or more inches for a man, counts as one “strike.”
What to do if you have this risk factor: Combine aerobic exercise, such as walking, jogging, cycling, or swimming, with muscle-strengthening activities, such as lifting weights or resistance training. Both types of exercise help dieters avoid regaining belly fat after weight loss, suggesting that regular workouts are essential for maintaining a healthy weight and waistline. Always check with your medical provider before starting a new fitness regime to make sure it’s right for you. Also ditch sodas and other sugary drinks: Drinking even one daily boosts risk for metabolic syndrome and diabetes by up to 20 percent! Coffee, on the other hand, lowers risk by about 13 percent, according to an analysis of studies that included nearly 160 million people. - High blood pressure. Recently, the American Heart Association and American College of Cardiology updated their blood pressure guidelines, with 130/80 mm Hg as the new threshold for a hypertension diagnosis, while systolic pressure (the top number) between 120-129 and diastolic pressure (the bottom number) below 80 is classified as “elevated.” Based on this definition, nearly half of U.S. adults — 116 million people — have hypertension. Medical criteria for metabolic syndrome, however, use a different blood pressure number: If your pressure is 130/85 mm Hg or higher, you have a “strike.”
What to do if you have this risk factor: Have your blood pressure checked regularly and talk to your provider if even one of your numbers is abnormal (a reading of 120/80 or above). Although medication is usually necessary to treat hypertension, there are also some natural ways to lower blood pressure. These include mindful meditation to reduce stress (an important contributor to elevated blood pressure); eating foods that are rich in magnesium (which helps regulate blood pressure), such as dark green leafy vegetables, unrefined grains, and legumes; and getting 7-8 hours of sleep a night (skimping on slumber is linked to increased risk for hypertension). - Low HDL cholesterol. HDL (high-density lipoprotein) is the “good” cholesterol. An HDL level below 50 mg/dL for women, and under 40 mg/dL for men, is another strike for metabolic syndrome. Many people who are headed for arterial disease and diabetes will run low HDL levels. If you are being treated for low HDL, you have a strike even if the levels are above 50 and 40 mg/dL.
What to do if you have this risk factor: if you use tobacco or nicotine in any form, here’s yet another reason to kick this deadly habit: Several studies link quitting to a rise in HDL levels. Eating oily fish (such as salmon, tuna and sardines) or other foods that are high in omega-3 fatty acids helps boost levels of good cholesterol while reducing inflammation. Olive oil is also a healthy fat that helps raise HDL. For an added benefit, use it to dress a salad with purple produce, such as red cabbage, blueberries, black raspberries or blackberries. These tasty foods contain disease-fighting antioxidants called anthocyanins, which have been shown to raise HDL by up to 19 percent in small studies. - High triglycerides. Like cholesterol, triglycerides are a type of fat found in your blood. When you consume more calories than you burn, the extra calories are converted into triglycerides and stored in fat cells until they’re needed for energy. In other words, when fat accumulates on your thighs or belly, that’s where excess triglycerides end up. If your triglyceride level is 150 mg/dL or above, you have acquired another strike. If you are being treated for high triglycerides, it is a strike even if the level is below 150 mg/dL.
What to do if you have this risk factor: If you’re overweight, losing 5-10 percent of your body weight (10 to 20 pounds if you weigh 200) can lower your triglycerides by 20 percent, according to the American Heart Association. Limiting or avoiding sugar, and increasing the fiber in your diet, also are helpful. Also ask your healthcare provider to check you for vitamin D deficiency. Among the many benefits of the sunshine vitamin is supporting healthy triglyceride levels. Multiple studies have linked low levels of vitamin D to increased risk for high triglycerides and metabolic syndrome. - High fasting blood sugar. Fasting means you have not consumed anything with calories for at least ten hours. A level of 100 mg/dL or higher counts as a strike. Fasting blood sugar levels of 100 mg/dL to 125 mg/dL indicate you’re prediabetic, while a level above 125 mg/dL is diagnostic of diabetes. If you don’t know your blood sugar numbers, ask your provider to check them, preferably with the two-hour oral glucose tolerance test rated as the gold standard in accuracy for diabetes screening.
What to do if you have this risk factor: To prevent or reverse prediabetes, the treatment that surpasses all others is aerobic exercise, such as running, brisk walking, biking or swimming. Working out 30 minutes daily, five or more times a week, has been proven to prevent prediabetes from progressing to full-blown diabetes 60 percent of the time, while the success rate rises to 70 percent if regular exercise is combined with moderate weight loss (5-7 percent of your body weight), large studies report.