March 16: Weekly COVID-19 Update, Volume 3
If you are one of the millions of Americans who takes angiotensin converting enzyme inhibitors (ACE-I) or Angiotensin Receptor Blockers (ARBs) to treat high blood pressure, diabetes or heart disease, or have friends or relatives who do, please read and share this important patient alert from the Heart Attack & Stroke Prevention Center and the BaleDoneen Method. False and misleading claims circulating on social media allege that these commonly used medications may raise both the risk of infection and the severity of COVID-19. In reality, there is NO scientific evidence to support these claims — and some evidence that ACE-I and ARB medications may actually PROTECT against serious lung complications in people with COVID-19, according to a position statement issued by the European Society of Cardiology (ESC) on March 13.
These alarming claims, which have also appeared in tabloid newspapers, have frightened some patients into stopping their ACE-I or ARB medications and others to ask their medical providers if they should switch to other blood pressure medications. In response, leading experts from the ESC’s Council on Hypertension “strongly recommend that physicians and patients should continue treatment with their usual anti-hypertensive therapy because there is no clinical or scientific evidence to suggest that treatment with ACE-I or ARBs should be discontinued because of the Covid-19 infection [emphasis added by the ESC].”
The BaleDoneen Method, which has long used ACE-I and ARBs as cornerstones of our evidence-based treatment of arterial disease to help our patients avoid heart attacks and strokes, concurs with this advice. We also strongly emphasize that patients should NOT stop ANY prescribed medications unless advised to do so by their medical providers. Here is what every patient who takes ACE-I or ARBS needs to know.
What are ACE-I and ARB medications — and why are they prescribed?
ACE-I and ARBs are types of renin-angiotensin aldosterone system (RAAS) inhibitors. This system regulates blood pressure and the body’s fluid balance. RAAS inhibitors reduce the effects of angiotensin, a hormone that constricts blood vessels and raises blood pressure. By causing these vessels to relax and widen, these drugs lower high blood pressure, the leading risk for stroke. Since angiotensin also promotes blood clotting and can contribute to arterial wall inflammation, it is not surprising that numerous studies show that medications that reduce the effects of this hormone lower heart attack and stroke risk.
Indeed, the scientific evidence is so overwhelming that in 2004, the American College of Physicians recommended this type of medication for all patients with coronary artery disease (CAD). The BaleDoneen Method goes one step further and prescribes these medications to patients with plaque in any of their arteries, not just those that supply the heart. To us, it doesn’t make sense to focus solely on heart attack prevention (by solely treating people with CAD) and ignoring those with plaque in their neck arteries that could lead to a devastating stroke. RAAS inhibitors have also been shown to shrink risk for cardiovascular events in people with blood pressure as low as 110/70. ACE-I and ARBs both target the same process that constricts blood vessels, but each inhibits or blocks a different step in the process, as follows:
- ACE inhibitors. These medications prevent an enzyme called ACE2 from converting the substance renin into angiotensin. The ACEs are the oldest type of RAAS inhibitors and have a wealth of studies showing significant reductions in heart attacks, strokes, heart failure and kidney failure. Examples of ACE-I include Accupril (quinapril), Aceon (perindopril), Altace (ramipril), Capoten (captopril), Mavik (fosinopril) and Vasotec (enalapril). Ramipril has superior data on outcomes, with the very large HOPE study reporting a 32 percent drop in risk for strokes, 20 percent for heart attack, 26 percent for cardiovascular fatalities and a 34 percent decrease in new cases of diabetes. No other ACE has been shown to be nearly as effective for preventing diabetes — a very important benefit for patients with arterial disease, since many of them are prediabetic.
- Angiotensin receptors blockers. One drawback of ACE-I is that in about 10 percent of patients, these medications can cause a dry, hacking cough. If this occurs, we switch our patients to an ARB medication, such as Benecar (Olmesartan) or Diovan (valsartan). As the name suggests, ARBs block the action of angiotensin by preventing it from binding to receptors in blood vessels and other tissues, much as filling the lock on your front door with cement would make your house key useless. ARBs significantly lower stroke risk but do not lower heart attack danger. They are also effective for preventing and treating heart and kidney failure, with very few side effects. They help prevent diabetes, but not as effectively as ACEs.
What’s behind the claim that these medications raise risk for COVID-19 infection and severity?
Several tabloid newspapers have run articles with such fear-mongering headlines as, “DRUG ALERT: Medicine taken by millions could increase the risk of getting coronavirus, scientists warn,” “Coronavirus: Blood pressure medication could worsen symptoms” and “High blood pressure and diabetes medication taken by 13 million Americans could raise the risk of serious coronavirus symptoms, scientists say.” These alarmist articles have been amplified on social media — literally “going viral” with highly unscientific, and false, claims.
The “scientists” cited in these headlines are the three European authors of a letter published in Lancet Respiratory Medicine on March 11. Their letter starts by stating, correctly, that Chinese studies of patients with COVID-19 report that it occurs at higher rates and with greater severity in people with heart disease, diabetes and high blood pressure. The letter’s authors then note that these conditions are often treated with ACE-I — then admit that none of the studies they cite looked at whether or not any of the patients studied were actually taking these medications! Nor do the authors mention that COVID-19 also occurs at increased rates and with worse outcomes in people with cancer and chronic respiratory disease, neither of which is treated with ACE-I or ARBs.
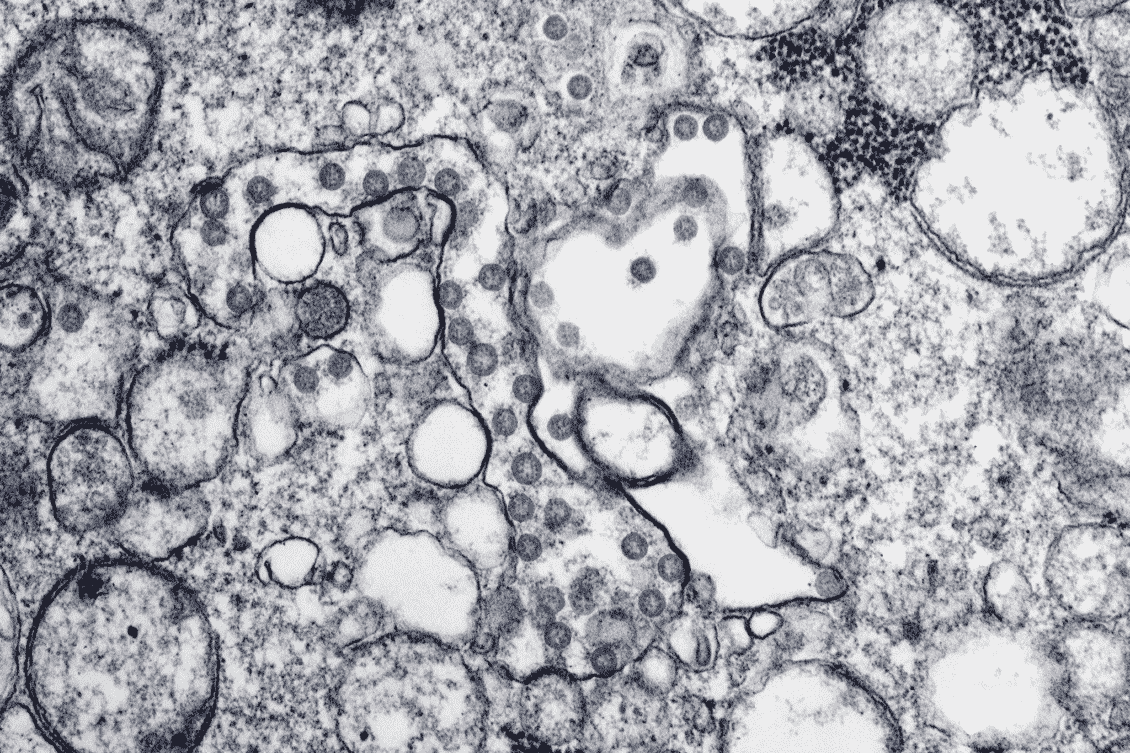
The letter also states, accurately, that coronavirus binds to receptors for ACE2, an anti-inflammatory pathway in the RAAS pathway. The authors then take a wild leap by speculating (with NO scientific evidence whatsoever) that people who take ACEs and ARBs might be more vulnerable to the virus, because these drugs block an inflammatory pathway called ACE1, leading to an increase in ACE2 receptors. The authors then go even further, again with NO scientific evidence, and hypothesize “that diabetes and hypertension treatment with ACE2-stimulating drugs increases the risk of developing severe and fatal COVID-19.”
The letter concludes by suggesting that patients be switched to other types of blood pressure medications, even though these do not offer the proven and potentially lifesaving cardiovascular benefits of ACEs and ARBs. Nor do these alternative medications prevent type 2 diabetes, a disease that greatly increases risk for heart attacks, strokes and many other complications, especially if it goes undiagnosed and untreated.
What’s the evidence suggesting that ACEs and ARBs might PROTECT against severe COVID-19 lung complications?
In response to the fear-mongering headlines and social media posts the Lancet letter has provoked, ESC’s council of hypertension experts from numerous European cardiology societies states, “This speculation about the safety of ACE-I or ARB treatment in relation to COVID-19 does not have a sound scientific basis or evidence to support it. Indeed, there is evidence from studies in animals suggesting that these medications might be rather protective against serious lung complications in patients with COVID-19 infection, but to date there is no data in humans.”
The research the ESC statement cites is titled, “[RAAS] inhibitors are one of the possible options for treating the new coronavirus pneumonia” and was published in the Chinese Journal of Tuberculosis and Respiratory Medicine in February. The key findings of the study are:
- COVID-19 is combined with human ACE2 infection to produce severe pneumonia, which is highly contagious and has a high mortality rate.
- RAAS inhibitors might be a good choice for treating COVID-19 pneumonia, which does not yet have an effective, precise therapy.
- COVID-19 creates an imbalance of the RAAS system, by decreasing ACE2 and increasing ACE1, leading to inflammation and pneumonia.
- Therefore, ACE-I and ARBs could be used to reduce ACE1 in patients with COVID-19, which in turn might reduce the pulmonary inflammatory response and death rate.
- Imbalances of ACE1 and ACE2 — and variations in the distribution of ACE2 in people who develop COVID-19 — may explain why some patients, especially children, develop mild symptoms, such as stuffy nose, sore throat and diarrhea, while others rapidly develop complications, such as severe pneumonia and septic shock.
In response to claims that ACE-I and ARBS might put people at higher risk for COVID-19 infection and severe illness, the study points out that children and young adults naturally have significantly HIGHER levels of ACE2 than do elderly people. Yet, as of this writing, there are NO published reports of children dying from COVID-19. All studies to date suggest that most children infected with the virus either develop mild illness or no symptoms at all, while older people (who naturally have lower levels of ACE2) are at the greatest risk for severe illness.
The study suggests that ACE or ARB medications could be considered as potential treatment for COVID-19, combined with close monitoring of blood pressure. The researchers report that this is likely to be an effective strategy to reduce body damage in patients with COVID-19. Therefore an additional potential benefit of being on an ACE or ARB, if it’s prescribed for high blood pressure, diabetes or heart disease: as possible protection against severe pneumonia, one of the most dangerous manifestations of COVID-19.
Again, we emphasize that the European Society of Cardiology and the BaleDoneen Method strongly recommend that patients who are being treated with ACE or ARB medications continue with their current blood pressure treatment and not let social media updates or tabloid headlines scare them away from potentially lifesaving medications that have been proven in numerous studies to protect against heart attacks, strokes and other complications of arterial disease and/or high blood pressure. Please share this update widely to help us debunk the false claims circulating online and help us save lives, brains and hearts through evidence-based treatment!
Where can you learn more about COVID-19 and heart or circulatory disease?
For tips on how to protect yourself and the latest news about COVID-19, read our blog posts, “Coronavirus: How Concerned Should You Be?” and “Covid-19: What Every Patient with Heart Disease Needs to Know.” Also check out our blog post, “The New Blood Pressure Guidelines: 4 Things to Know” and “The Number One Risk for Stroke—and What to Do About It.” Additional resources include the following:
- American Heart Association: “What heart patients should know about coronavirus.”
- CDC: “Coronavirus Disease 2019 (COVID-19)”
- CDC: COVID-19, If You Are at Higher Risk
- Heart Matters: “Coronavirus: what it means for you if you have heart or circulatory disease.”
- Johns Hopkins: “Coronavirus Interactive Map”
- Johns Hopkins: Coronavirus Resource Center
- New England Journal of Medicine: Coronavirus (Covid-19)
- Harvard Health: Coronavirus Resource Center